November SonoProps
This month’s SonoProps goes to Dr. Nina Vazquez (who hadn’t even started her ultrasound rotation yet) and Dr. Erin Gonzalez.
Dr. Gonzalez had an 85-year-old female that was brought in by EMS as stroke alert for acute onset left sided weakness and disorientation. She took no medications and was otherwise healthy reportedly. There was no prior history of stroke or heart disease. Easy right? CT/CTA, maybe TPA, admit to stroke neurology, done. Not so fast!
After a thorough physical exam, Dr. Gonzalez asked Dr. Vazquez to perform an echocardiogram as she had suspicion this wasn’t just a stroke. I was working at the same time so Dr. Gonzalez and I supervised Dr. Vazquez’s POCUS exam.
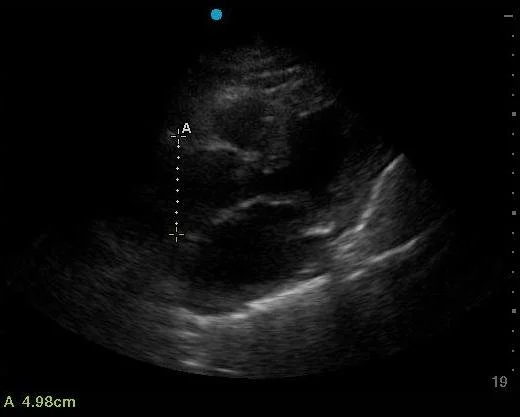
Here is what we saw:
Can you identify what the abnormality is? Think about the next best step. Here is an an additional view that was obtained.
What view is this? What can you identify here that is abnormal?
The finding in the second image above is very subtle - it is a still from the first clip above. This highlights the importance of knowing clinically, all the signs and symptoms of the pathology you are looking for as well as the ultrasonographic characteristics. The dilated aortic root alone should give you a hint.
This patient had a Type A Aortic Dissection that caused a stroke, would not want to TPA that at all! The patient was accepted by CT surgery and admitted.
The first clip shows a very dilated aortic root, as measured 4.98cm (>4cm is considered abnormal for the thoracic aorta/aortic root).
The second clip is a suprasternal view demonstrating a dissection flap. In the second image, there is indeed a VERY subtle dissection flap that shows up only for a second in the first clip.
Learning points:
Signs of aortic dissection on POCUS echocardiography include:
A dilated aortic root/thoracic aorta >4cm.
A visible dissection flap.
Aortic regurgitation
A new pericardial effusion in the setting of high suspicion for dissection.
Atraumatic hemothorax (new pleural effusion, again in the setting of high suspicion for dissection).
TTE alone may be insufficient to diagnose dissection with a reported a sensitivity of 67-90% and a specificity of 71-100% for this diagnosis, however it can rule IN the diagnosis. CTA is the test of choice, with TEE being a potential second option.
Regional wall motion abnormalities may be present, suggesting occlusion of the coronary arteries from a dissection flap. Stroke symptoms may be present if the dissection flap extends up the carotids.
The second SonoProp goes to Dr. Daniel Herzog and Dr. Vivek Sharma!
The reason for this particular SonoProp is their use of a technique I like a lot.
Dr. Herzog had a patient with a history of diabetes and hypertension who presented to the emergency department with a foreign body sensation in his right 3rd finger. The finger was mildly swollen with no erythema or fluctuance. Dr. Herzog made excellent use of our ultrasound resident at the time Dr. Sharma and this what they saw:
They used a hand water bath to scan the patient’s finger and definitively visualized a retained foreign body that could not be seen just on physical exam.
Using an 18-gauge needle the foreign body was easily removed.
The second clip is post procedure, note the absence of the hyperechoic foreign body. Excellent follow through study.
Learning points:
Water baths can be used for extremity ultrasounds. Water is an excellent acoustic conductor and will give great images. Using gel on extremities may allow poor contact and also uses pressure which may cause patients pain or discomfort. Water baths eliminate those issues. Water baths are also potentially an excellent technique for pediatric patients to avoid radiation and minimize discomfort.
Some pathologies that may be evaluated using water baths include:
Foreign bodies (as above)
Felons
Flexor tenosynovitis
Osteomyelitis
Tendon injuries
Vascular lesions
Fractures
Demonstration of a water bath.
Fill a bucket with water to cover the limb. Float the transducer as deep or shallow as necessary to obtain views. Obtain at least two views in transverse and sagittal orientation.