August SonoProps
The first SonoProps goes to Dr. Evan Feinberg!
Dr. Feinberg evaluated a 16-year-old male patient with dyspnea with exertion as well as right-sided chest discomfort.
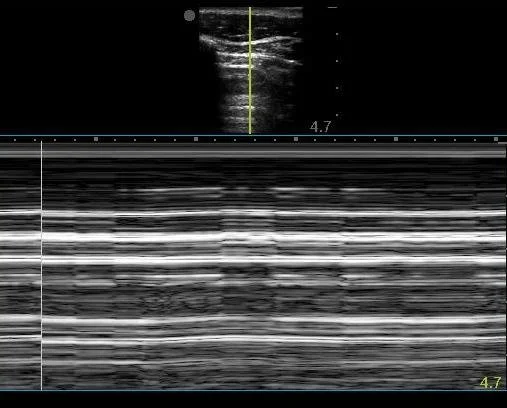
The patient had this interesting ultrasound finding:
This image very clearly demonstrates the “Barcode sign” on M-mode, which indicates absent lung sliding.
Normal lung sliding produces a "Sandy beach" or "Seashore" sign.
The first clip demonstrates no lung sliding on the patient’s right. Note the left side shows normal lung sliding with normal small comet tail artifact.
Learning Points:
Absent lung sliding most commonly is due to a pneumothorax, but be aware there can be false positives, namely:
Prior pleurodesis (or other causes of lung adherence like malignancies)
Right mainstem intubation (if you check the lungs post-intubation) or tumor in a mainstem bronchus
ARDS (and extremely high PEEPS)
Phrenic nerve injury/palsy
Blebs in COPD (“bleb point”)
Pleural malignancies or inflammatory pleural conditions
Absence of lung sliding is very sensitive for detection of pneumothorax, but specificity is around 78-80% with PPV of 57%, NPV 100%.
If you see lung sliding, you have ruled out pneumothorax at that point, but if you don’t see lung sliding, look for other signs of pneumothorax such as lung point to rule in pneumothorax. Lung point may be found by moving the the transducer laterally to find the location where the visceral pleura loses contact with the chest wall. Lung point is purportedly 100% specific for pneumothorax. Also, correlate with history and the patient’s clinical stability. The presence of B-lines excludes pneumothorax at that point as B-lines require a pleural sliding interface.
The second SonoProps goes to Dr. Gabriel Struck.
Dr. Struck evaluated a 49-year-old female with abdominal pain, the patient was not pregnant. She hypotensive and tachycardic (.notsepsis). Dr. Struck grabbed the ultrasound machine and saw this on his scan:
The patient was resuscitated and taken the OR where she had 2 liters of hemoperitoneum evacuated and had a TAH, BSO, radical cytoreductive surgery, bladder resection and repair, placement of suprapubic Foley, resection of small bowel and ascending colon with ileotransverse anastomosis for suspected ovarian cancer.
Learning Points:
You might think that FAST/FAFF (Focused Assessment for Free Fluid – the generic non-trauma term) is mostly valuable in suspected pregnant patients after the last SonoProp but FAFF has a role in any hypotensive patient.
A FAFF exam can provide valuable information regarding the abdomen as a source for hypotension. The abdomen can hold a significant amount of blood.
There are many sources of intraabdominal bleeding to consider in a male or non-pregnant female.
Causes of non-traumatic hemoperitoneum have been grouped into etiologies such as:
Iatrogenic (related to prior surgery, intervention, or anticoagulation)
Tumor-related
Gynecological
Vascular
The three most common causes among women and in decreasing frequency are: ruptured ovarian cyst (women < 35 years old), recent procedure, and unknown mass.
In this case a gynecological tumor was the source of hemoperitoneum. Depending on the patient’s exam, you can choose to start with the FAFF or a quick cardiac exam to evaluate for hypotension.
Remember, a negative FAST/FAFF exam does not rule out pathology, but it does help to state there is no free fluid/hemoperitoneum, it is a rule IN test. The next steps should be to get a CT or to perform serial FAST/FAFF examinations depending on your goal.