May SonoProps
Spring is in the air, and so is another edition of SonoProps! You all are not making it easy for me and there were a number of excellent scans this month.
Our first SonoProps goes to Dr. Erin Gonzalez and Dr. Obioma Nkemakolam!
There was basically no way I could NOT give them a SonoProps for this scan…
They had a 64-year-old male referred to the emergency department from their primary care doctor for new rapid atrial fibrillation. The patient’s blood pressure on arrival was normal and the patient was in rapid atrial fibrillation to the 160’s.
Easy, Cardizem and admit the patient right?
Not so fast… Dr. Nkemakolam and Dr. Gonzalez are POCUS-users. They don’t sit back waiting for answers, they make the answers come to them!
They did a POCUS echo and saw the following —
Not just rapid atrial fibrillation!
This is a massive pericardial effusion, measuring up to 5.0cm in it’s largest portion. There are signs of tamponade on this echo — aside from the obvious “swinging heart,” there is right ventricular diastolic collapse. The right ventricle does not get a chance to fully fill during diastole due to the extra-cardiac pressure from the pericardial effusion.
Diagnosis: Extra-large pericardial effusion with a side of tamponade
The patient had 1500ml of serosanguinous fluid drained by cardiology.
Learning points:
New arrhythmias of any kind of should prompt a POCUS echo. You may be surprised at what you may discover and significantly impact patient care. If this patient had not gotten a POCUS echo, who knows how long the diagnosis of massive pericardial effusion with tamponade would have taken to diagnose.
Atrial arrhythmias have been associated with pericardial effusions (28774768).
Basic features of cardiac tamponade on ultrasound include right atrial systolic collapse, right ventricular diastolic collapse, a plethoric IVC, and a mitral inflow variation >25%.
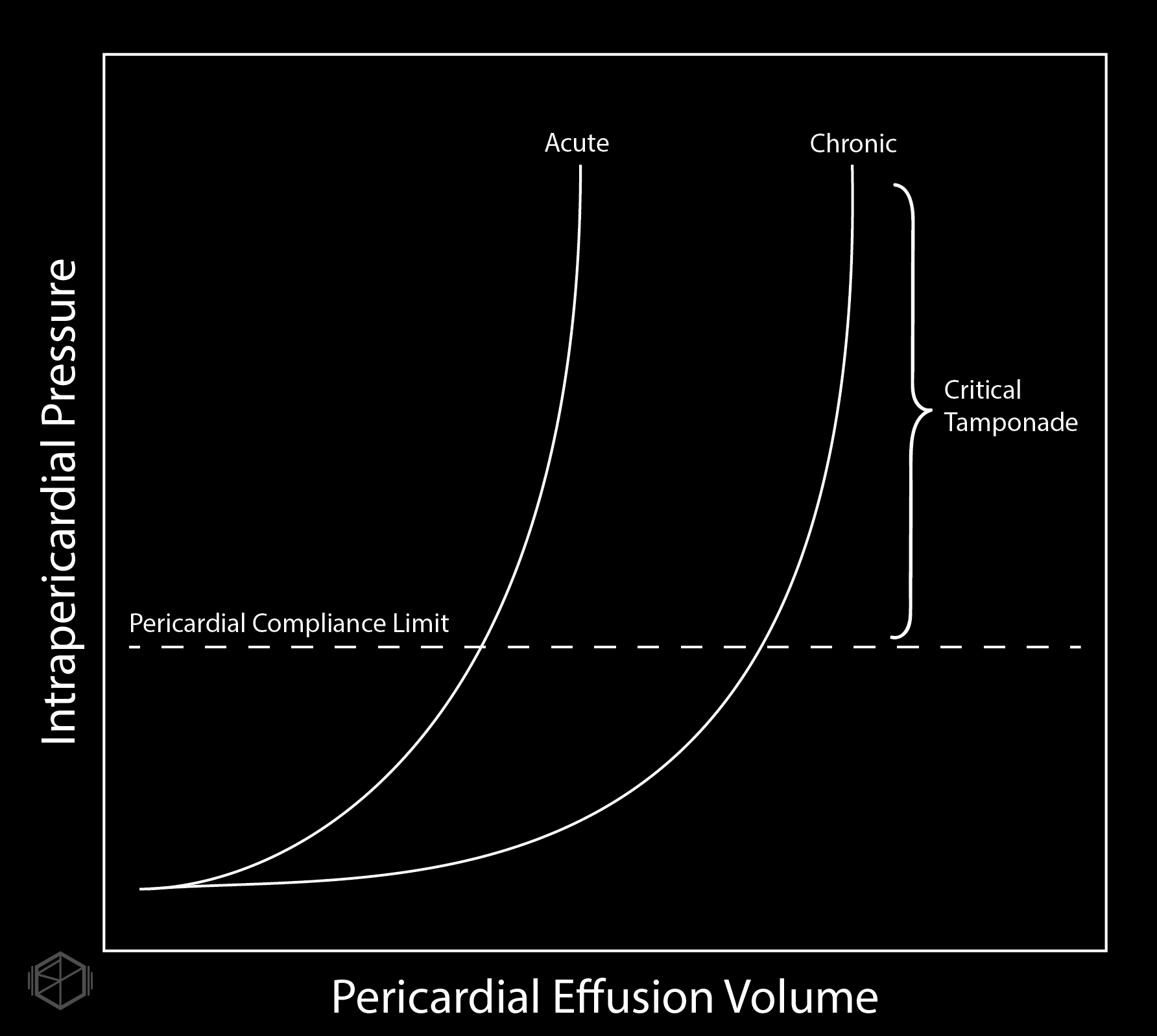
The acuity of pericardial fluid accumulation matters more than the size of the fluid. Large pericardial effusions can be tolerated if gradually developed.
The next SonoProp goes to Dr. Herzog and Dr. Nkemakolam.
They had a 77-year-old male presenting to the ED complaining of shortness of breath. The patient had a history of CHF and multiple episodes of pneumonia. He was tachypneic, tachycardic, and hypoxic. The team did a POCUS of the lungs and saw the following.
This patient has B-lines, but note the irregular pleural borders that appear jagged. These are subpleural consolidations. In the correct clinical context, subpleural consolidations are a sign of infectious process although they can also be found in other pathologies as well.
Diagnosis: Multifocal pneumonia
Learning points:
In adults, lung ultrasound also has a high sensitivity and specificity, with a high likelihood ratio for diagnosing pneumonia. (38299193, 26107512, 21030550).
Subpleural consolidations are irregularities in the pleural lining that appear jagged.
Subpleural consolidations can be an indication of pneumonia (viral or bacterial), but are also found in other pathologies such as pulmonary embolism (eg, infarcted lung). Correct clinical context and an examination of the heart using POCUS can be helpful to help distinguish the two pathologies.
The presence of focal B-lines and subpleural consolidations has a high positive likelihood ratio for diagnosing pneumonia (29189351).
Shred sign or fractal sign — subpleural consolidation with highly irregular borders/shredded borders. B-lines usually surround the edge of the shred sign given pneumonia is a gradual fluid process that occupies airspace.